Partnership in prostate cancer; the feasibility of an integrated system to improve patient outcomes and experience (ICARE-P Study)
Project Su mmary:
mmary:
Prostate cancer is the most common cancer in men in the UK, and there are a large number of survivors with 85% of men diagnosed surviving for at least five years. Hospital-based services are over-stretched and recent guidelines emphasise a broadening role for the GP in providing follow-up care. GPs are well placed to address the range of patients’ needs, which may include psychological and social as well as physical concerns. In addition there is increasing recognition of the importance of sharing data between GP and hospital- based services and the potential of information technology to improve healthcare through rapid communication.
The aim of this study is to test the feasibility of undertaking a full trial to compare a new model of prostate cancer care with standard care. In this model, information technology provides a basis for the integration of care between the GP practice and specialist hospital services. This study is split into two phases, with Phase 1 consisting of qualitative interviews, and Phase 2 the non-randomised cluster RCT.
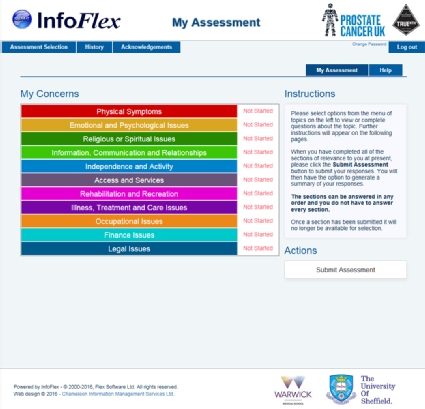
For this feasibility study, we will recruit men with a diagnosis of prostate cancer at any stage in the care pathway who have been treated or diagnosed at University Hospitals Birmingham. Participants will be recruited from GP practices that refer patients to UHB. We have recruited 14 practices, of which 10 will be in the intervention group that tries out the new approach. Practice nurses at these surgeries will take part in specialised training. Men recruited from the 10 practices will complete an online self-assessment: the Holistic Needs Assessment (HNA), before having a consultation with their practice nurse to discuss any problems identified by the assessment. This will occur three times at six month intervals. Participants in the control group will have their care as usual, and all participants will complete measures to assess quality of life, symptoms and use of health care services at baseline, and 9 months later. The results from this study will be used to analyse how the HNA is used by men over a 9 month period and to refine the methods and design of a large scale trial to investigate outcomes for patients and clinical and cost effectiveness.
The research team is:
University of Warwick
Dr Veronica Nanton (Principal Investigator)
Miss Rebecca Appleton (Research Associate)
Prof Theo Arvanitis (Professor of E-Health Innovation)
Prof Jeremy Dale (Professor of Primary Care)
Mr Thomas Hamborg (Medical Statistician)
External
Prof Sam Ahmedzai (University of Sheffield)
Mr Douglas Badger (User Representative)
Mr Peter Smith (Patient Representative)
Dr Richard Mendelsohn (Birmingham South Central Clinical Commissioning Group)
Mr Prashant Patel (University Hospitals Birmingham NHS Foundation Trust)
Professor Nick James (University Hospitals Birmingham NHS Foundation Trust)
Dr Richard Mendelsohn (NHS Birmingham South & Central CCG)
Mr Marc Warburton (IT Consultant - CIMS)




